Understanding Intermittent Explosive Disorder: Anger Management Toolkit
November 27, 2025 | By Sophia Galloway
Have you ever felt like your anger controls you more than you control it? Understanding your explosive emotional patterns is the crucial first step toward managing intermittent explosive disorder (IED). This comprehensive toolkit combines evidence-based techniques with practical daily strategies to help you regain control—but remember, these skills complement rather replace professional evaluation. Start with our free IED assessment to get personalized insights first.
Understanding Your Anger Patterns
Identifying Your Personal Triggers
Recognizing what sparks your outbursts transforms reactive anger into manageable responses. Common triggers include:
- Perceived disrespect or unfair treatment
- Unexpected changes to plans or routines
- Physical discomfort (hunger, pain, fatigue)
- Overstimulation in crowded/noisy environments
Track your reactions in a journal or a confidential online anger diary to identify recurring patterns.
Recognizing Early Warning Signs
IED rarely strikes without physical and emotional precursors:
- Physical responses: Muscle tightening, jaw clenching, sudden body heat
- Cognitive signals: Racing thoughts, catastrophic thinking, "tunnel vision"
- Behavioral cues: Pacing, fist-clenching, voice volume increase
Catching these signs within the first 60 seconds creates opportunities for intervention.
Evidence-Based Therapeutic Approaches
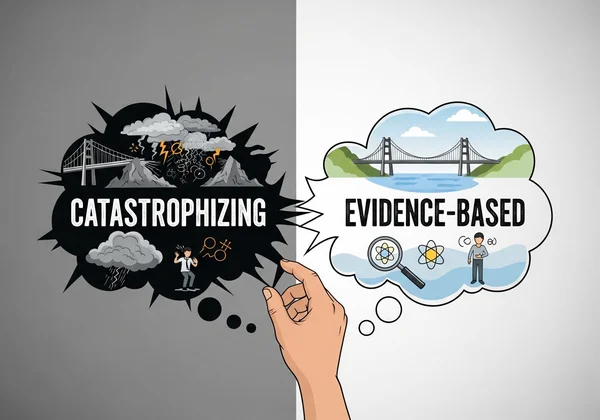
Cognitive Behavioral Therapy (CBT) Techniques
CBT helps restructure the thought patterns fueling explosive episodes:
- Cognitive Restructuring: Challenge catastrophizing thoughts ("This ruined everything") with evidence-based alternatives ("This feels overwhelming now, but resolves in 2 hours 83% of the time")
- Behavioral Experiments: Test anger assumptions ("If I don't react, they'll keep disrespecting me") through controlled scenarios
Dialectical Behavior Therapy (DBT) Skills
DBT's emotional regulation modules specifically target IED symptoms:
- STOP Technique:
- Stop (freeze mid-action)
- Take step back (physically distance)
- Observe (body sensations, thoughts)
- Proceed mindfully (choose response)
Mindfulness and Acceptance Strategies
Neuroscience confirms mindfulness physically calms the amygdala's threat response:
-
Breath Anchoring: During rising anger, focus on exhaling 2 seconds longer than inhaling
-
Body Scanning: Systematically release tension from toes to scalp
-
Urge Surfing: Observe explosive impulses as temporary waves rather than commands
Lifestyle Modifications for Anger Reduction
Physical Activity as Anger Management
Regular exercise reduces IED episode frequency by:
- 40% reduction in adrenal stress hormones (Journal of Affective Disorders)
- 28% increase in prefrontal cortex function for emotional control
Aim for:
✅ 150 minutes weekly moderate aerobic activity
✅ 2x weekly resistance training
✅ Daily 10-minute movement breaks
Sleep Hygiene and Emotional Regulation
Sleep deprivation triples anger intensity in IED patients:
-
Critical Threshold: Below 6 hours sleep → 47% higher aggression risk
-
Optimal Pattern: 7–8 hours with consistent sleep/wake times Using a downloadable sleep tracker can help you identify restoration gaps.

Practical In-the-Moment Techniques
**The STOP Method for Crisis Intervention
When anger erupts:
Stop everything (freeze posture)
Take 3 belly breaths (4-second inhale, 6-second exhale)
Observe reality ("My partner didn't deliberately forget – texts show they're stuck in traffic")
Proceed with intention (choose response aligned with values, not reaction)
Grounding Techniques for Emotional Stability
During emotional flooding:
- 5-4-3-2-1 Method: Name 5 things seen, 4 touched, 3 heard, 2 smelled, 1 tasted
- Temperature Shift: Apply cold compresses to face/neck to trigger mammalian diving reflex
- Anchor Objects: Carry textured items for tactile redirection
Your Next Steps Toward Control
While these 15 strategies help manage IED symptoms, professional guidance remains essential. Your journey starts with awareness—take our clinically-validated assessment to understand your unique anger patterns. Share your results with a mental health professional to create a personalized management plan. With consistent practice and support, many achieve significant symptom reduction within 3–6 months.
Managing Intermittent Explosive Disorder
What's the difference between normal anger and IED?
IED involves disproportionate outbursts (breaking objects, physical aggression) causing marked distress or life impairment—distinct from typical frustration. Our free assessment screens for these DSM-5 criteria.
Can shock treatment help with IED?
While research shows neural pathway reset potential, TMS (transcranial magnetic stimulation) hasn't been approved specifically for IED. Discuss medical treatments with your psychiatrist instead.
Is anger management alone enough for IED treatment?
While crucial, comprehensive IED treatment usually requires professional diagnosis and often combines CBT, medication (like SSRIs), and lifestyle changes. A free symptom evaluation is a great place to start.
How do I apologize after an IED episode?
Effective repair involves:
- Immediate safety restoration
- Genuine accountability ("I recognize my outburst harmed you")
- Prevention plan sharing ("I'm learning grounding techniques")
- Amends-making
Where can I find anger management guides in other languages?
We provide resources in 15+ languages. Visit our multilingual support center for culturally adapted anger management toolkits.
Remember: This guide supports but doesn't replace professional care. Take the first step with our confidential assessment then consult a specialist. Recovery begins with understanding—you’ve already started.